Abstract
Introduction: Sickle cell disease (SCD) is the most common genetic blood disorder, affecting an estimated 100,000 people in the US and over 20 million worldwide. SCD costs one and a half billion dollars of economic loss annually in the US, resulting in sustained burden to the families and the healthcare systems (Value in Health 2021;24:1095). Many patients living with SCD require frequent blood draws and may have to have a central line for routine blood draws. A blood hemoglobin (Hgb) level is the central information about the pathophysiology of SCD including anemia. Low blood Hgb levels have shown as a potential indicator of painful vaso-occlusion crises (Blood 2021;137:2010). Blood Hgb levels are checked for evaluation of new symptoms, medication monitoring, and routine follow up. Real-time and noninvasive monitoring of blood Hgb levels would be clinically beneficial, but less feasible through frequent invasive blood draws. Developing a reliable, self-educated, and completely non-invasive mobile health (mHealth) tool for real time blood Hgb assessments can directly benefit many patients living with SCD, minimizing the number of iatrogenic blood loss from frequent blood draws and improving the quality of care.
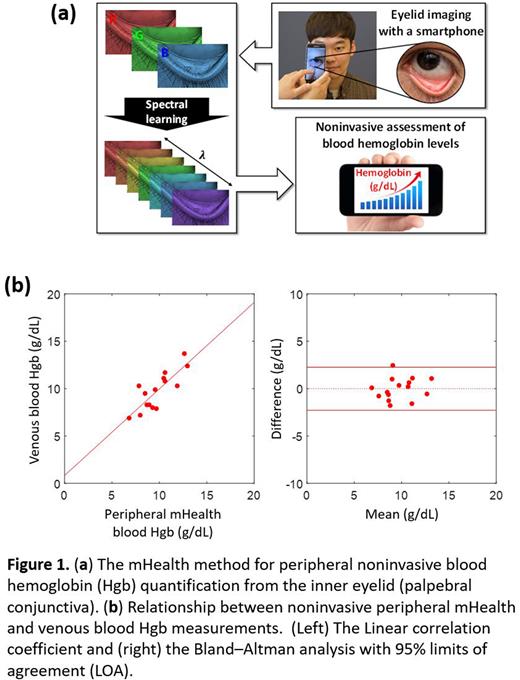
Methods: Our team has recently developed an mHealth algorithm that can reliably estimate a blood Hgb level from a photo of a peripheral tissue site at individual's inner eyelid (palpebral conjunctiva) (Figure 1a). We conducted a pilot study to determine the exact relationship between peripherally detected blood Hgb levels (accessed from the inner eyelid) and blood Hgb tests (venous blood draws) performed at a clinical laboratory. Fifteen patients with SCD aged from 14 to 73 years were recruited at Hematology Clinic at University Hospital of the Indiana University School of Medicine. Acquisitions of the inner eyelid photos in RAW format were conducted by Samsung Galaxy S21 immediately before or after a blood draw. Blood Hgb levels from the inner eyelid's photo were computed using the previously developed statistical learning algorithm (Optica 2020;7:563); the first step was to recovery a spectrum from an RGB image (spectral learning) and the second step was to compute blood Hgb content using a spectral analysis (Figure 1a).
Results: The linear correlation between the peripheral mHealth blood Hgb levels and the venous blood Hgb levels in the blood (i.e., the gold standard) shows a value of 0.82 with a p-value of 0.0002 (Figure 1b). A Bland-Altman analysis was also conducted as a non-parametric statistical method. The limits of agreement (LOA) were defined by a 95% prediction interval of the standard deviation of the differences between the mHealth and conventional blood Hgb levels. 95% Bland-Altman LOA was +/-2.3 g/dL (Figure 1b) and within LOA, the data points were uniformly scattered, indicating no significant bias. This level of performance is comparable to point-of-care blood sampling (finger prick) testing and noninvasive medical devices (Respiratory Care 2019;64:1343).
Conclusion: This preliminary study supports the feasibility of peripheral and noninvasive mHealth blood Hgb assessments among patients with SCD. Importantly, peripheral mHealth blood Hgb levels are significantly associated with conventional venous blood Hgb tests among SCD patients. Thus, the mHealth technology can lay the groundwork for empowering individual patients by offering an easily accessible tool for quickly estimating blood Hgb levels by a smartphone. This mHealth technology has potential advantages including mobility, simplicity, and affordability for rapid and real-time blood Hgb quantification among patients living with SCD.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.